+1 804 221 1273
Why We Are Cash Pay
INSURANCE CREATES BARRIERS*
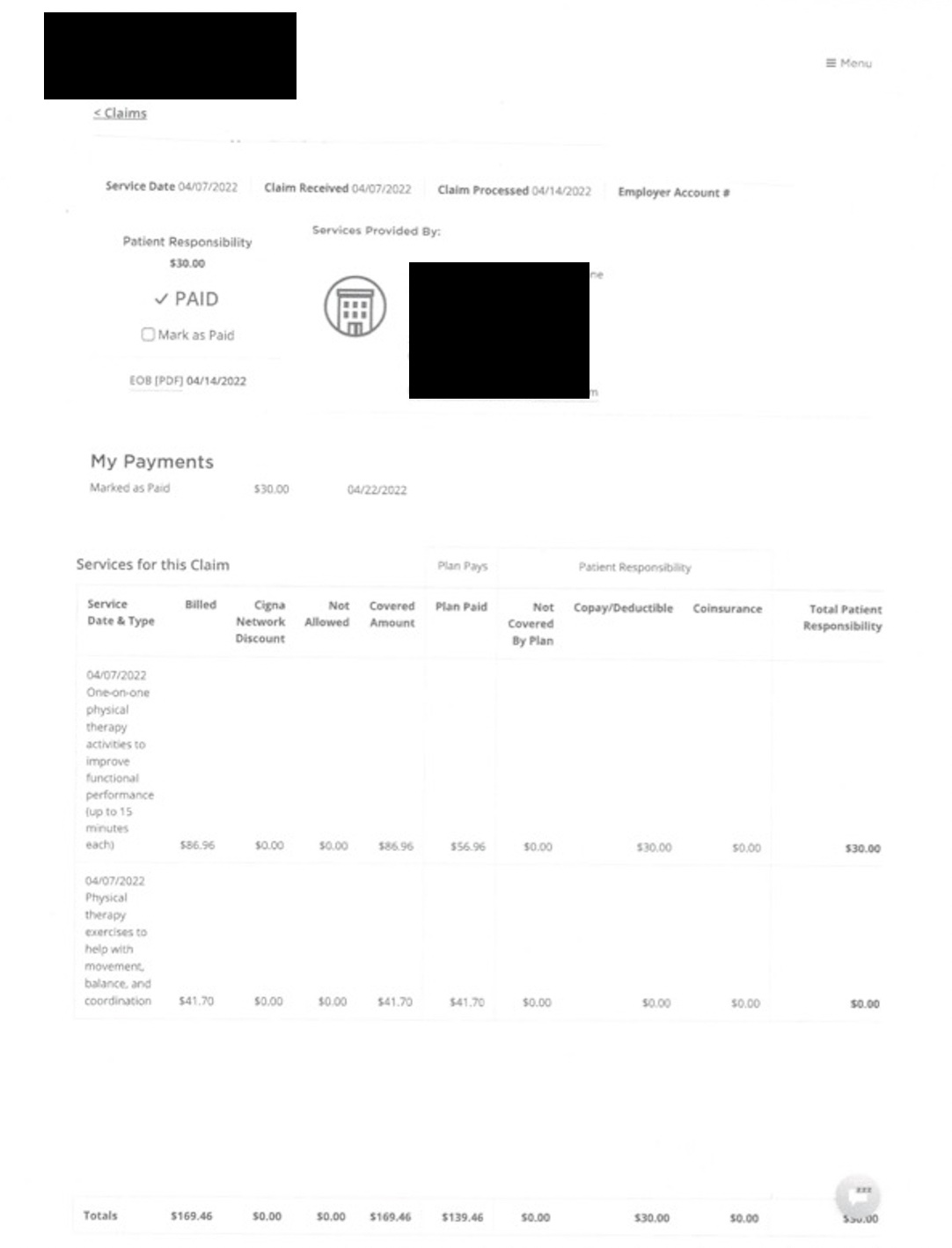
To your right is a sample Estimation of Benefits (EOB) from a national insurance plan. I have the patient's consent to post this as an opportunity to discuss insurance and how it works as an example of why cash pay is critical for long term success.
With this plan at the corporate facility I worked at, I usually billed her for 60 minutes. I spent a dedicated half-hour with her as the PT and then I worked with another patient or two while I was directing her with some exercises planned out in advance. She did a lot at home and was very compliant so often we did 30 minutes of hands on therapy since she was a post achilles tear and repair and at this point she was 5 months out and was unable to complete any rigorous PT for 3 months.
We had to be very judicious as her insurance plan works by requesting authorization in advance. That gave us a limited amount of visits, very careful documentation, and making sure timeframes were met. For instance, we had a set plan of care where she had to come 2x a week for 4 weeks, whether she could or not, or we had to ask for an extension because insurance dictated what they would cover and when.
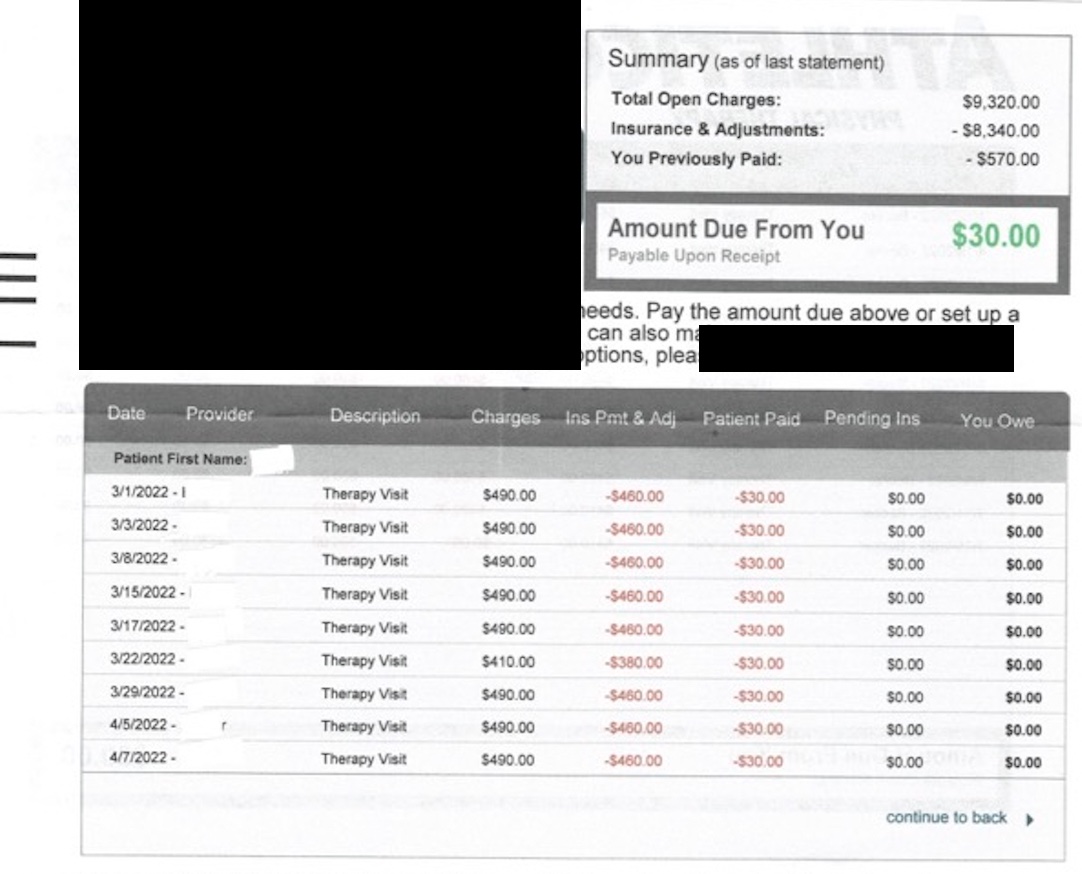
UP FRONT COSTS MEANS NO SURPRISE BILLS
You can see on the bill that the normal amount charged was for $490 for one date of service. Even though the allowed reimbursement per unit billed is $40 [a unit = 15 minutes] - the PT company billed more than $150 (which would be for the 4 units). This amount can be higher or lower depending on your plan deductible and insurance allowable charges which vary based on contracts between your insurance and each provider. Often you do not know the actual costs until you get your first bill - and that could be a month or longer into your sessions.
Her insurance did not have a deductible, but if your plan does (as most do) you might end up being responsible for 100% of the cost of these visits + the $30 co-pay until your deductible is met (a total of $520!).
If you owed 20% co-insurance on an 80/20 plan until your deductible as met you would owe $98 + the $30 copay for EACH VISIT.
Here at AAPT you know your costs up front and you have the freedom to choose which monetary amount/sessions work best for you.
1:1 CARE = BETTER PATIENT OUTCOMES
All of these scenarios are for sessions where the therapist sees you for at most 30 minutes. At Arts and Athletics Physical Therapy I can provide you the same treatment, but for an hour of one-on-one care without other patient interruption for a max of $100 an hour of treatment.
CUSTOMIZED CARE
You can also choose to come 1x/week or 1x/month. Insurance does not get to dictate a plan of care or a therapist who is trying to meet productivity requirements by asking you to come 3x a week. This can save you both time and money.
As you saw in the previous section three times a week with her plan would be $90 in copays alone weekly - not counting any potential additional charges. At AAPT you can chose the length of your sessions based on what you need- maybe once a week for 15 minutes at $25/week, or twice a week for 45 minutes at $150/week. But no surprise bills - ever.
FREEDOM FROM VISIT LIMITS
My former patient actually had a great insurance plan, but even hers had limits - such as when they tell you they will only cover 6 visits after major surgery because the plan allows for 20 total visits and no one told you you already used 14 during your treatment to see if PT would help and then 6 more visits while you were waiting to get an MRI or other imaging approved. Or you already used those visits treating a different injury earlier in the year. That is potentially 18 visits gone before you even had imaging.
At AAPT we are not limited by insurance's rules/policies so whether you need care for months after surgery or periodic check-ins every few months you can truly live a life without limits.

WE WANT YOU BETTER -
GUARANTEED
At Arts and Athletics Physical Therapy we have a 6 visit guarantee.
If you are not feeling better in 6 visits then we will work with you and your medical team to help you achieve your results in the best way possible.